Roland Berger advises pharma, MedTech and insurance companies on how to master the challenges of the future.

Health insurance apps: an opportunity for differentiation
By Karsten Neumann and Nils Breuer
What apps can do and how they need to be designed so that health insurance companies retain customers and win new ones
In all areas of life, more and more activities are shifting to digital channels. Health insurance companies (SHI and private health insurance) have also recognized the benefits of apps for communicating and exchanging information with policyholders. Many are already using them - not least to increase their efficiency and reduce process costs. At the same time, the aim is to attract new users and increase the frequency of use in order to achieve economies of scale.

But what services do policyholders expect to find in their health insurance app? Which are frequently used, which are less relevant? And what can be deduced from the different expectations of the individual target groups for the future direction of the offering?
To find this out, we conducted a representative study asking around 1,000 SHI and 200 private health insurance policyholders about their individual preferences for digital services relating to administration, prevention or care and the user experience of existing services.
"User-friendly apps open up great opportunities for health insurance companies to differentiate themselves from the competition."
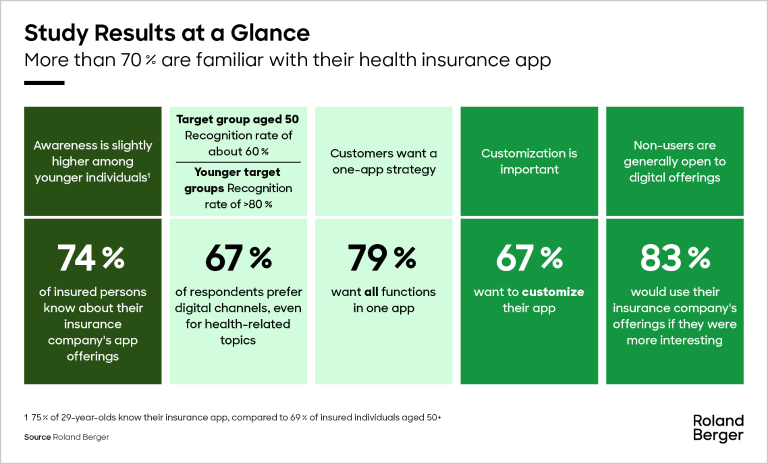
Policyholders prefer digital channels that are easy to use
As the results show, many policyholders are very interested in digital offerings - even if only 30 percent have used their insurer's app to date. For example, 74 percent of participants stated that they were aware of their insurer's digital front ends. Two thirds even prefer digital channels to analog ones when it comes to dealing with their concerns. The preference for digital solutions is particularly pronounced among younger respondents up to the age of 29. However, more than 80 percent of those who do not yet use them are also open to attractive offers.
There are various reasons why the apps are not currently being used more frequently. For a quarter, these include a lack of information about the benefits and functionality of the app, but also a lack of user-friendliness (19 percent) and problems with registration and login (15 percent). In the eyes of many younger people, the user interface and controls in the app are also not attractive enough.
Insured persons who already use their health insurance company's app do so primarily to carry out administrative tasks - for example, to make an appointment with a doctor or to check the current status of their bonus program. The ability to store contact information for emergencies and to query health data are also cited as important functionalities. Simple services that make the insured person's everyday life easier are preferred. The fact that the app combines all central services in one application is at least as important to policyholders as a clear and easy-to-find presentation of the desired services and information.
Specifics of different target groups offer opportunities for app expansion
The results clearly show that the interests and needs of insured persons differ greatly according to age and marital status. Health insurance companies can make targeted use of these differences when expanding their digital offerings.
For the target group of young and digitally savvy policyholders, the focus should be on services such as medication reminders or telemedicine services. Fast and efficient handling of their administrative tasks is a relevant and attractive added value for this target group. Families, on the other hand, are particularly interested in solutions for managing family health. They are also attracted to the app with the help of bonus programs and prevention offers. In our survey, almost half (46 percent) stated that they were interested in information on children's health and preventive care. Health insurers could address this desire by expanding the administrative functions for parents, for example by automatically reminding them of their children's preventive appointments.
As our survey shows, the introduction of the electronic patient record (EPR) could give new impetus to the topic of insurance apps. As soon as the ePA can be filled with information and data, 75 percent of users see it as a suitable place where documents can be bundled and individualized treatment information can be retrieved. In the eyes of policyholders, this is also the biggest advantage of the ePA.
"Acceptance of digital services is high - even among non-users. Over 80% of those who do not yet use an app are open to digital services if the added value is clearly communicated."
The vision: The app as a health and communication center
Almost eight out of ten policyholders would like all of their health insurance's digital services to be bundled in one app (one app approach). To achieve this, however, the architecture of the applications must be fundamentally revised. The aim is to create a platform that is flexible, scalable and, above all, tailored to the needs of users. This is made possible with the help of layered logic. In such models, an application is divided into different layers, for example for content, functions or customer data. Each layer covers a specific task area and enables simple separation, but also adaptation of content and services.
With a One App approach that comprehensively addresses the wishes of the target group and offers policyholders access to integrated service modules via a central account, health insurance companies can gain important competitive advantages. The aim must be to establish the app as a central platform for health management that offers policyholders the opportunity to track their health data, manage appointments and communicate with other healthcare providers. By offering personalized recommendations and reminders, it also supports care management, optimizes patient care and improves the efficiency of the healthcare system.
Register now to access the full German publication „Krankenversicherungs-Apps: Eine Chance zur Differenzierung“. Furthermore, you get regular news and updates directly in your inbox.
_person_144.png?v=1034513)



_person_320.png?v=1034513)

_person_320.png?v=1085250)