This healthcare survey in GCC, focusing on KSA & UAE. Explore the shift to value-based care, population priorities, and key findings for impactful reforms.

The future of population health management
By Sara Barada, Tara Makarem, Oussama Nicolas and Elsy Dumit
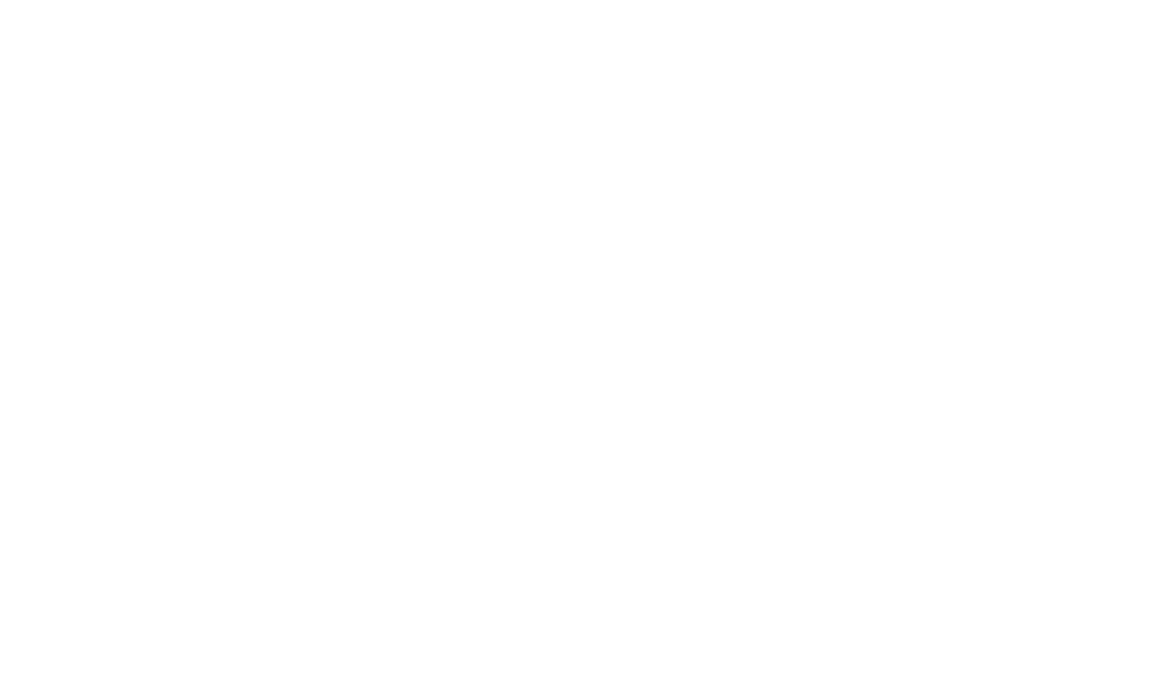
Population Health Management (PHM) stands at a transformative juncture, shaped by rapid technological advancements and new scientific discoveries. At Roland Berger, we envision a near future where cutting-edge technology and science work together to support individuals in realizing their maximum health potential.

This article delves into how integrating cutting-edge technology and scientific research in PHM models can ultimately lead to improved health outcomes, with a particular focus on addressing the unique health challenges and opportunities within the GCC region. By moving away from reactive health measures to a proactive, predictive, precise, participatory, and personalized health system, we aim to empower individuals and systems alike to manage and preempt health challenges and advance, maintain and expand populations’ healthy life span.
Proactive Population Health Management (PHM) from gestation
PHM typically involves identifying, segmenting, stratifying, and targeting high-risk populations based on their service utilization and demographic factors. It aims to apply public health and healthcare interventions to improve health outcomes. However, we believe that the journey of PHM can begin even earlier — before birth.
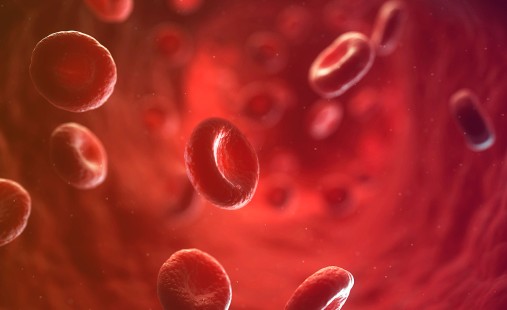
From the time of gestation, the health system can gain a comprehensive understanding of the genomic characteristics of individuals-to-be by utilizing advanced genetic testing and broader "-omics" applications. This helps identify specific genetic markers that indicate an increased risk for various health conditions, such as asthma or congenital heart defects. Additionally, environmental factors — including maternal nutritional intake, exposure to pollutants, and the mother’s home address — are monitored to assess their impact on the health of the developing fetus, as these factors directly affect the mother.
Understanding genetic predisposition and exposure to risk factors enables healthcare providers to implement targeted interventions for both mothers and their children. This may involve limiting certain environmental exposures and following strict dietary guidelines for mothers. These measures aim to minimize the potential impact of health issues and support the mother's and child's overall well-being from the earliest stages of life.
"Imagine the power of converging of ethically-driven science, technology and human will on the future of Population Health Management and its impact on enabling people to live longer healthier lives."
Smart 360-degree monitoring in real-time
As individuals grow, their health, behaviors, social interactions, and environmental exposures are continuously monitored in a smart, real-time, 360-degree manner, while accounting for data privacy/regulations and adopting a balanced approach for public health surveillance. Currently, PHM focuses primarily on monitoring clinical data to assess an individual's health status. However, clinical factors account for only 20%¹) of what influences a person's health, while lifestyle and environmental (non-biological) factors comprise the remaining 80%¹). We define "360-degree monitoring" as the continuous collection and analysis of data related to wider determinants of health, including social, economic, behavioral, environmental, and clinical information, to develop a well-rounded understanding of individuals' health status.
IoT devices and wearables track vital signs, physical activity, sleep patterns, and dietary habits / nutritional information in real-time. At the same time, advanced sensors evaluate environmental conditions, such as air quality and noise levels. Data on social and community interactions is also collected to provide a comprehensive view of each person's living conditions and support systems. Other emerging technologies are now also coming into play, such as fridge sensors to identify lifestyle factors.
Advanced health analytics tools examine a vast amount of data to identify patterns and potential health risks that might not be immediately apparent. A 360-degree monitoring approach offers a holistic view of individuals' health and well-being by incorporating various aspects of health and environmental factors.
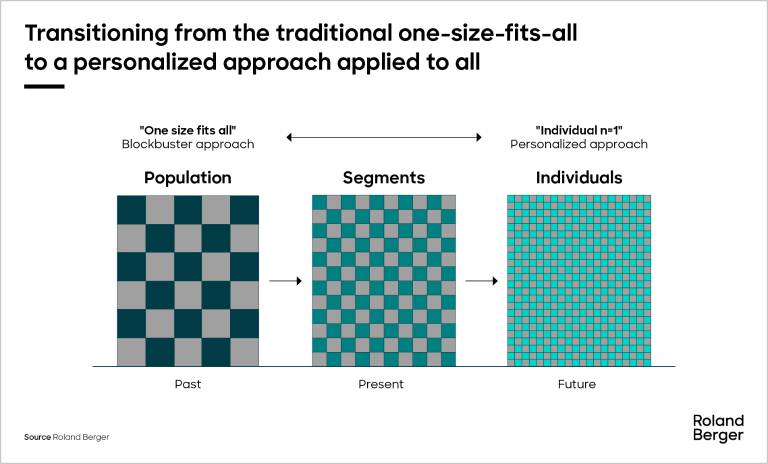
Individualized population segmentation at n=1
Traditional PHM typically groups individuals into broad categories based on general factors such as age, gender, medical history, and healthcare service utilization. However, this approach can overlook the unique nuances of each individual's health profile. With the wealth of information gathered through 360-degree smart monitoring, we can achieve a new level of individualized population segmentation. This approach moves away from traditional population segments and instead views each person as a unique entity, employing a population segmentation strategy at the n=1 level.
By collecting data on each individual, we can create a digital twin or virtual replica that captures genetic, physiological, behavioral, social, and environmental aspects using Big Data analytics and machine learning. Using sophisticated predictive modeling and multi-variable risk stratification supported by Big Data analytics and machine learning, allow us to identify individuals at higher risk for specific diseases. For example, a person with a genetic predisposition to heart disease who is also exposed to environmental pollutants and leads a sedentary lifestyle can be flagged for close monitoring and early intervention.
By segmenting the population at the individual level, healthcare providers and health workers can design personalized interventions that are precisely tailored to each individual’s needs.
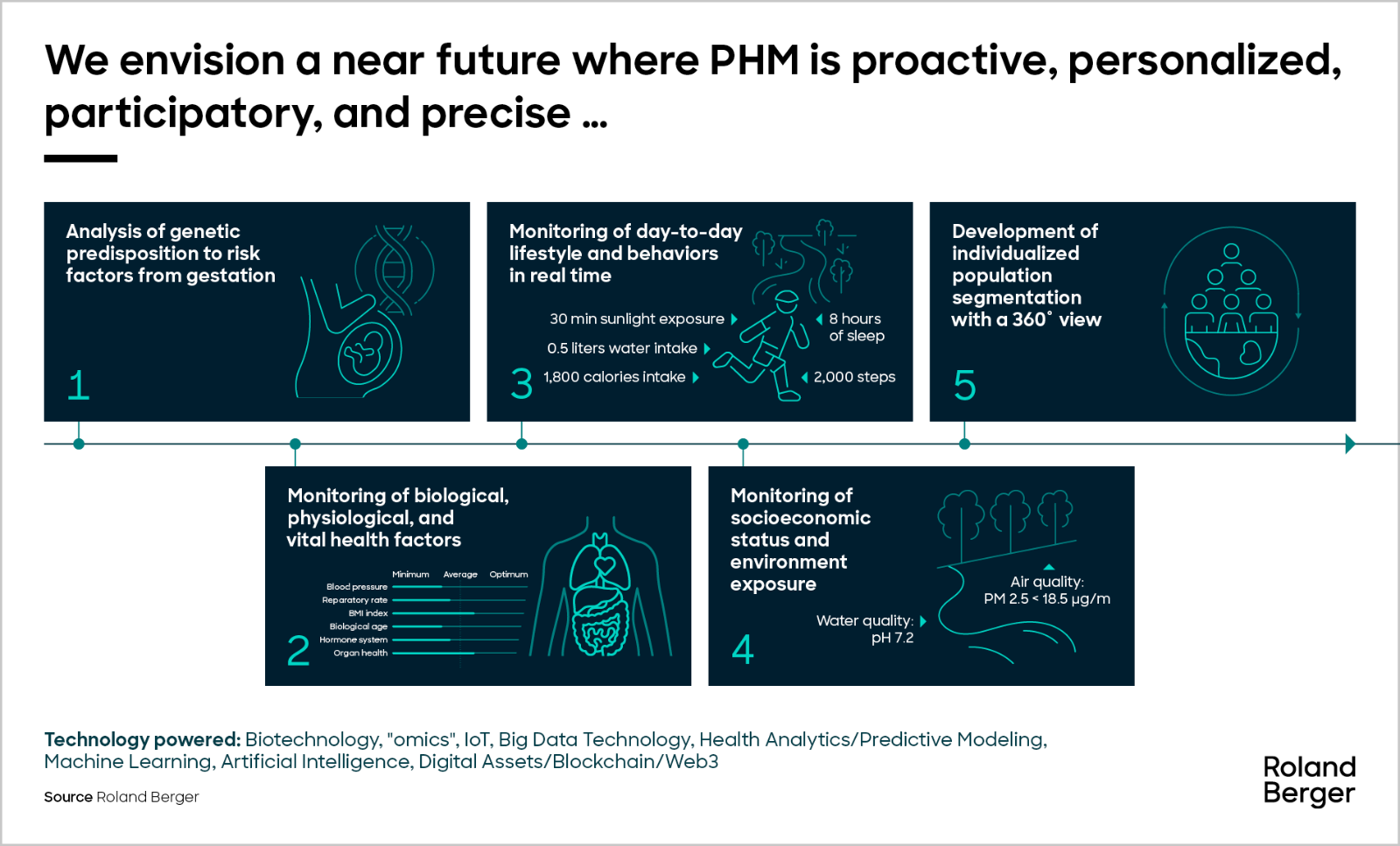
Personalized and targeted preventive interventions
Building on this individualized segmentation approach, key healthcare stakeholders (i.e., regulators, providers, payors, etc.) leverage understanding of individuals at the n=1 level to tailor preventive and healthcare interventions while also introducing real-time digitally empowered “nudging” techniques based on real-time exposure to risk factors to maximize individuals’ health potential.
Predictive modeling and AI tools play a crucial role in this process, continuously analyzing health data and simulating scenarios using digital twins to identify the right intervention at the right place and at the right time. Individuals can also be proactively nudged to alter their behavior on a day-to-day basis, to better comply with a treatment regime, or to seek care or preventive services such as regular check-ups and screening when needed.
Consider a middle-aged man with a BMI of 30 and a sedentary lifestyle. Through predictive modeling, the individual can be flagged as having a high risk of developing type 2 diabetes. A customized dietary plan can then be developed, tailored to the individual’s lifestyle and preferences, considering their preferred foods, allergies, and place of residence. The health intervention is pushed to the individual using targeted channels to maximize adoption potential, all while monitoring the individual’s response and adherence to the dietary plan.
This dynamic, real-time approach helps preventive measures be effective and sustainable, thus helping individuals maintain their health over the long term.
Learning system and continuous impact monitoring
PHM focuses on ongoing improvement and adaptation to enhance the health and well-being of individuals while optimizing the overall health of the population. By utilizing AI and machine learning algorithms, health outcomes are monitored, and data on individual responses to interventions, personal values, and preferences are analyzed. This process helps refine strategies, identify the most effective approaches for each person, and adjust their health plans. Continuous monitoring of these impacts ensures that health management remains dynamic and responsive, adapting to new insights and evolving circumstances.
Integrating digital models allows for simulating various health scenarios to optimize outcomes. These models also serve as effective population activation tools, enabling individuals to visualize the impact of different health interventions and lifestyle choices and fostering their active participation and engagement. By understanding the potential benefits of adhering to a specific health plan or the consequences of neglecting it, individuals are more likely to take proactive steps to maintain their health and “stick to” to new and improved lifestyle behaviors.
The continuous monitoring and analysis of health data form the foundation of this futuristic Population Health Management model, creating an evolving learning system for constant improvement.
Case for PHM in the GCC and way forward
a. Current situation in the GCC
The Gulf Cooperation Council (GCC) health systems face various challenges, including clinical, behavioral, social, and environmental factors that impede progress in population health outcomes and elevate healthcare costs.
Non-communicable diseases (NCDs), such as diabetes, cardiovascular diseases, and cancer, are leading causes of mortality in the region. For example, diabetes affects over 18%²) of the population in Saudi Arabia, while cardiovascular diseases account for nearly 20%³) of all deaths in the UAE. Although communicable diseases like tuberculosis and hepatitis are less prevalent, they still pose risks, especially among migrant populations in countries like Qatar and the UAE.
Behavioral factors significantly contribute to the rise of NCDs. Poor dietary habits, low levels of physical activity, and smoking are linked to obesity, diabetes, and heart disease. Nearly 40%⁴) of adults in the GCC region are physically inactive, and childhood obesity rates exceed 45%⁵) in several countries. This situation increases the likelihood of chronic diseases developing earlier in life.
Social factors, such as urbanization and changing lifestyle patterns, worsen the region’s health issues. The increased availability of fast food and processed meals, coupled with more sedentary lifestyles, is particularly prevalent in major urban areas.
Environmental factors, particularly air pollution, are also a major contributor to health issues in the region. For example, the average annual concentration of particulate matter (PM2.5) in Riyadh⁶) is estimated to be around 80 µg/m³ and 76 µg/m³ in Doha⁷), more than three times the World Health Organization’s (WHO) recommended limit of 25 µg/m³. The high levels of PM2.5, along with similar air quality issues in cities like Riyadh, greatly increase the risk of respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD).
Together, these clinical, behavioral, social, and environmental factors are driving healthcare costs higher. In the GCC, the current health expenditure (CHE) is estimated to have grown at a compound annual growth rate (CAGR) of 9.5% from 2020 to 2022, reaching USD 104 billion⁸). It is expected that this expenditure will increase further to USD 135.5 billion in 2027. To tackle these challenges, a comprehensive PHM approach is needed, focusing on prevention and long-term health outcomes.
b. Emerging PHM efforts in the GCC
In recent years, GCC countries have begun to embrace PHM initiatives, driven by a unique combination of regional health trends, economic goals, and demographic factors. These include the prevalence of NCDs such as cardiovascular diseases, obesity, and diabetes, which rank among the highest globally. Additionally, the rising costs of healthcare—exacerbated by NCDs, an aging population, and inflation—are a significant concern. There is also a pressing need to improve healthcare access in remote and rural areas. Furthermore, the GCC must manage the health of a large expatriate population alongside local citizens. Moreover, the region faces unique challenges during mass gatherings, particularly in Saudi Arabia during the Hajj and Umrah seasons, which require robust health management strategies. These factors collectively underscore the critical need for effective PHM systems in the region.
GCC countries have made progress in implementing components of PHM, particularly in addressing key health challenges such as NCDs and promoting healthier lifestyles. For example, Saudi Arabia's Vision 2030 emphasizes preventive health measures, including large-scale screening programs for diabetes and hypertension aimed at early detection. Similarly, national health campaigns in the UAE encourage residents to engage in daily physical activity to reduce the incidence of chronic diseases.
These initiatives often focus on specific health issues instead of adopting a fully integrated PHM model. Preventive health measures typically target individual conditions rather than acknowledging the interconnectedness of clinical, behavioral, social, and environmental health determinants. While this approach may yield short-term results, it falls short in creating a coordinated system for long-term and sustainable health management.
GCC countries can transition from isolated public health interventions to a proactive, comprehensive, data-driven population health management model that integrates prevention, personalized care, and health management.
c. Way forward to fuel PHM transformation in the GCC
Implementing a successful PHM model in the GCC requires several key enablers, including regulatory reforms, infrastructure development, technology integration, and a shift in mindset. To establish a comprehensive PHM model in the GCC, it is essential to address several critical enablers:
- Policy and regulatory support: Developing policies that promote value-based care, population health management, and secure and integrated health data sharing across the healthcare ecosystem
- National health governance: Designing data and clinical governance structures that align public and private key health ecosystem stakeholders to support cohesive PHM strategies
- Funding and investment mobilization: Structuring financial incentives, redesigning payment models that integrate population-level health outcomes, and fostering public-private collaborations to drive innovation and accelerate the adoption of PHM solutions
- Underlying data and technology infrastructure: Developing national exchange platforms that allow for secure, standardized data sharing, enabling effective decision-making and coordination
- Telemedicine and remote monitoring: Expanding telemedicine infrastructure to enhance care access, particularly in remote areas, with real-time health tracking capabilities
- AI and predictive analytics: Implementing AI-driven predictive models to identify at-risk populations, enabling targeted preventive interventions
- Preventive genomics: Advancing the field of genomics (and epigenetics) for prevention and PHM to build a stronger scientific foundation that promotes adoption and acceptance of such services among the population
- Social and environmental determinants: Addressing underlying social and environmental factors, such as air quality, physical activity, and nutrition, to enhance PHM effectiveness
- Community engagement strategies: Delivering public health campaigns and interventions that focus on people activation, encourage preventive care, foster sustained behavioral change, and promote the use of health technologies
- Shifting mindset to support PHM: Shifting healthcare professionals’ mindset to champion PHM approaches to health and equipping them with the skills to use advanced medical and digital health tools to deliver personalized, preventive care
d. Role of stakeholders in implementing PHM transformation
Collaboration among regulators, payors, providers, and individuals is essential for developing a sustainable and effective PHM model in the GCC.
Regulators establish the groundwork by creating policies and regulatory frameworks that promote value-based care, encourage standardized data sharing, and ensure patient privacy. Their role also involves fostering an environment that supports innovation in health technologies while accounting for the social and cultural impact of the future PHM model.
Payors, including both private insurers and publc payors, play a crucial role in promoting PHM by incentivizing preventive and proactive care instead of episodic treatment, thus aligning reimbursement models with long-term health outcomes.
Healthcare providers play a crucial role in implementing PHM by integrating preventive services, enhancing the population’s health literacy, and creating personalized care pathways. They utilize digital tools to proactively manage people’s health effectively.
Individuals also play an essential role as active participants in their health journey. Through population activation and engagement, communities are empowered to adopt healthier behaviors, participate in preventive interventions, and utilize health monitoring technologies.
Furthermore, IT and data providers play a crucial role in developing the digital platforms, AI-driven tools, and analytics necessary to support PHM. Meanwhile, community organizations and educational institutions help raise awareness and advocate for healthier lifestyles.
By collaborating, these stakeholders can create a proactive and cooperative PHM ecosystem that enhances health outcomes for the population, reduces costs, and promotes a healthier future for the GCC.
Conclusion
The future of Population Health Management is promising, with the potential to transform and extend healthier lives. By embracing scientific and technological advancements and integrating them into our health systems, we can detect and prevent diseases before they occur. This approach helps alleviate the burden on healthcare systems, promotes long-term health and well-being, and ultimately improves individual health outcomes while optimizing the use of healthcare resources.
This innovative approach not only enhances individual health outcomes but also promotes a healthier and more resilient population prepared to tackle the challenges of the future. By adopting a proactive, predictive, personalized, participatory, precise, and continuously adaptive health management strategy, we can build a healthcare system that is more efficient and effective. This will pave the way for a healthier future for everyone.
Our view of the future of PHM at Roland Berger aims to enhance individual health outcomes and contribute significantly to healthcare systems' sustainability in the GCC. By embracing innovation and forging a path toward smarter health management, we anticipate the future and actively create a healthier, more resilient society.
Roland Berger provides comprehensive support in the development and implementation of your Population Health Management aspirations. Reach out to us today to start your journey
Sources:
¹ University of Wisconsin Population Health Institute and Robert Wood Johnson Foundation: County Health Rankings
² International Diabetes Foundation: Saudi Arabia
³ World Health Organization - Global Health Estimates: United Arab Emirates
⁴ National Institutes of Health - Physical Inactivity, Gender and Culture in Arab countries
⁵ World Health Organization - World Obesity Federation: Prevalence of childhood overweight and obesity (%) in the Arab Gulf States
⁶ IQAir - Air quality in Saudi Arabia
⁷ State of Qatar Ministry of Development Planning and Statistics: Environment Statistics Report
⁸ Statista: Healthcare expenditures in the Gulf Cooperation Council from 2011 to 2027